Breast Thermography
Providing a risk assessment for a health condition offers a patient so much more than just limited disease detection. There are many conditions that currently have biomarkers that will warn far in advance of significant pathology. It is far better to warn of impending heart disease and diabetes than to suddenly find you have it and that significant damage has already been done. These risk markers give you time to make changes to either prevent the condition or at least control it. Thermography brings this same risk assessment to the breast health of every woman [4,5]. Not only can breast thermography warn that a cancer may be present, but also provide a marker of future risk along with a role in prevention [3-5, 10-12].
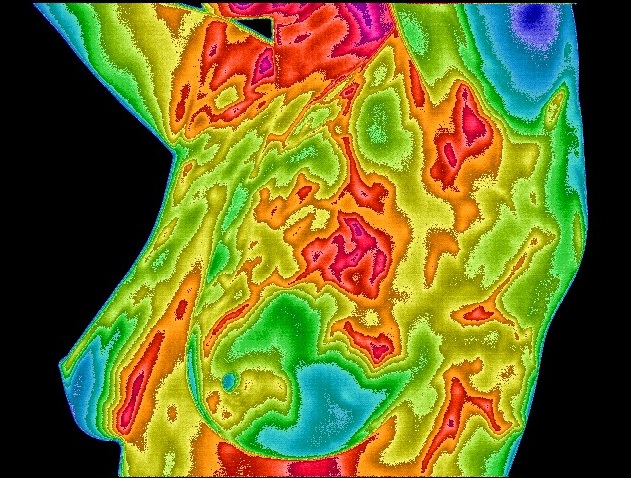
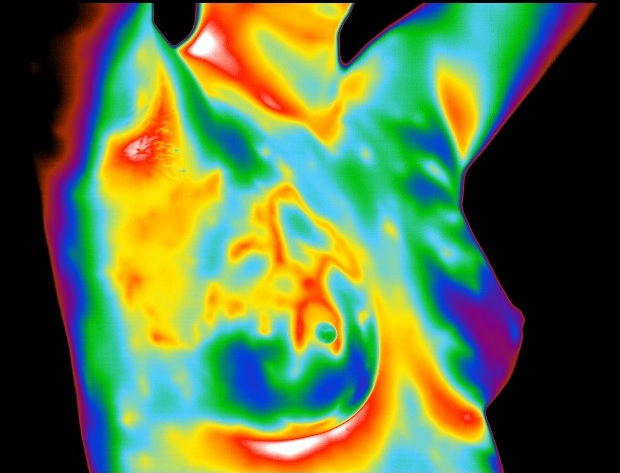
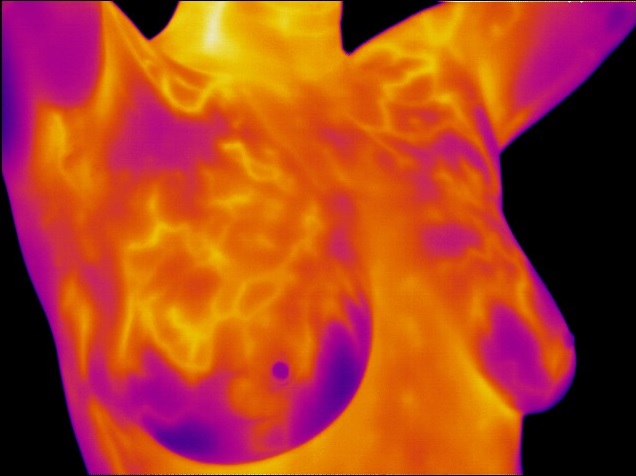
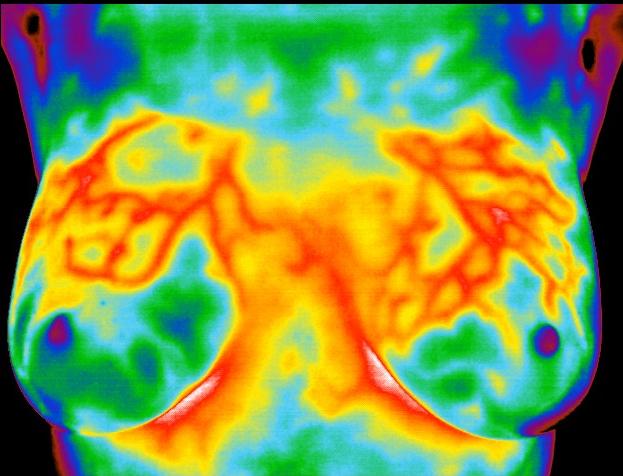
The use of thermography is based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue. In an ever-increasing need for nutrients, cancerous tumors increase circulation to their cells by holding open existing blood vessels, opening dormant vessels, and creating new ones (neoangiogenesis). This process frequently results in an increase in regional surface temperatures of the breast. Thermography uses ultra-sensitive medical infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution images of these temperature variations. Because of thermography’s detection ability, these temperature variations may be among the earliest signs of breast cancer and/or a pre-cancerous state of the breast [3,6-9].
Current methods used to detect suspicious signs of breast cancer depend primarily on the combination of both physical examination and mammography. While this approach has become the mainstay of early breast cancer detection, more is needed. Since the absolute prevention of breast cancer has not become a reality as of yet, efforts must be directed at detecting breast cancer at its earliest stage. As such, the addition of thermography to the frontline of early breast cancer detection brings a great deal of good news for women.
WHAT MAKES INFRARED IMAGING SO UNIQUE
While mammography, ultrasound, MRI, and other types of structural imaging rely primarily on finding the physical tumor, thermography is based on detecting the heat produced by increased blood vessel circulation and metabolic changes associated with a tumor’s genesis and growth. By detecting minute variations in normal blood vessel activity, infrared imaging may find thermal signs suggesting a pre-cancerous state of the breast or the presence an early tumor that is not yet large enough to be detected by physical examination, mammography, or other types of structural imaging [3,6-9].
Certain types of cancers will not be detected (approximately 20%) by mammography for various reasons [9], but some of these cancers will be discovered by thermography [3,6-9].
Difficulties in reading mammograms can occur in women who are on hormone replacement, nursing or have fibrocystic, large, dense, or augmented breasts (6,8). These types of breast differences do not cause difficulties in reading infrared images.
THERMOGRAPHY AS A RISK MARKER FOR BREAST CANCER
Studies show that an abnormal infrared image is the single most important marker of high risk for developing breast cancer, 10 times more significant than a family history of the disease [5]. Consequently, in patients with a persistent abnormal thermogram, the examination results become a marker of higher future cancer risk [4-5]. Depending upon certain factors, re-examinations are performed at appropriate intervals to monitor the breasts. This gives a woman time to take a pro-active approach by working with her doctor to improve her breast health. By maintaining close monitoring of her breast health with infrared imaging, self breast exams, clinical examinations, structural imaging, and other tests, a woman has a much better chance of detecting cancer at its earliest stage and preventing invasive tumor growth.
Angiogenesis, or new blood vessel formation, is necessary to sustain the growth of a tumor. Thermography may be the first signal that such a possibility is developing [3].
Just as unique as a fingerprint, each patient has a particular infrared map of their breasts. Any modification of this infrared map on serial imaging (images taken over months to years) may constitute an early sign of an abnormality. However, if a pathology is suspected, this information is used to recommend further examinations and tests.
THERMOGRAPHY’S ROLE IN BREAST CANCER PREVENTION
In another and possibly critical role, infrared imaging of the breast may hold a significant potential in breast cancer prevention. Due to the ability of infrared imaging’s detection of changes in the dermal circulation, any external pharmacological intervention or release of biochemicals by the body that have the propensity to alter blood flow may be detected. This is especially true of chemicals that are target specific for the tissues of the breast. Being a primary target tissue for the hormone estrogen, the hormone’s effect in the breast is anabolic to the ductal cells. As such, the outcome is one of increased cellular metabolism. This increase in cellular activity necessitates the need for nutrients above and beyond the norm. In order to facilitate this need, an increase in blood supply must occur. This translates to an infrared image demonstrating a uniform increase in vascular patterning (see images to the right).
The importance of this observation lies in one of the primary risk factors for breast cancer—lifetime exposure to estrogen. If infrared imaging has the ability to warn of increased thermovascular activity due to increased levels of estrogen in the breast (estrogen dominance), action can be taken to lower this activity and ultimately the patient’s risk for future breast cancer. Treatments can be monitored for positive effects by incorporating infrared imaging as a method of observing these effects. Studies have shown this effect and the positive outcome of pharmacological intervention. Many patients with this condition also demonstrate signs and symptoms that include breast pain, tenderness, cysts, and benign lumps. In many patients, a reversal or reduction in these signs and symptoms are also noted when treatment is initiated [10–12]. Infrared imaging’s ability to detect increased thermovascular activity secondary to levels of estrogen in the breast, and to monitor the effects of treatment targeted at the breast, may play a significant role in breast cancer prevention.
TECHNOLOGY, INTERPRETATION AND COMPARATIVE IMAGING
As is the case with mammography and all other imaging modalities, access to sophisticated technology and the expertise to interpret the findings are of prime importance. To help distinguish a normal process from an abnormal one requires proper training, clinical experience, strict adherance to guidelines and protocols, and meticulous image acquisition. While not all tumors are visible on a mammogram, not all tumors are associated with a high level of blood vessel activity; thus, escaping infrared detection. Less aggressive lesions can be associated with less evident images. Therefore, in these select cases, thermography may be an indicator suggesting a much better overall prognosis.
When digitally produced, and interpreted by qualified doctors, abnormalities or changes in infrared images provide invaluable information. This is particularly true in patients with dense breasts, non-specific physical or mammographic findings, or women with a previous history of breast surgery or radiation. The use of serial infrared imaging can draw additional attention to areas that require further evaluation or closer scrutiny during initial or subsequent exams. This further evaluation may include additional structural imaging. Used as a complimentary imaging technique, recent data suggests that thermography may also help monitor the effects of some of the newer proposed anti-angiogenesis therapies (currently recognized as a promising treatment strategy) [6,8].
Since we have not been able to prevent breast cancer as of yet, there is a consensus among experts that more lives will be saved with earlier detection. Since both physical and mammographic examination cannot detect all cancers, particularly smaller tumors in younger patients and those with dense breast tissue, there is currently much interest in finding new ways to improve our abilities in early detection. While some techniques have emerged, most are designed to be used in selected cases where physical and mammographic examinations have already picked up an abnormality. Consequently, we are left with some patients who have adhered to current screening guidelines and are still left with undetected breast cancer. Therefore, experts have concluded that no one procedure or method of imaging is solely adequate for breast cancer screening [1,2,6].
EARLY DETECTION MEANS LIFE
Breast cancer is the most common cancer in women, and the risk increases with age [1]. Risk is also higher in women whose close relatives have had the disease. Women without children, and those who have had their first child after age 30, also seem to be at higher risk. However, every woman is at risk of developing breast cancer. Current research indicates that 1 in every 8 women in the US will get breast cancer in their lifetime [1].
Studies show an increase in survival rate when breast thermography and structural imaging are used together [3].
Thermography’s ability to detect thermal signs that may suggest a pre-cancerous state of the breast, or signs of cancer at a very early stage, lies in its unique capability of monitoring the temperature variations produced by the earliest changes in tissue physiology (function) [3,6-9]. However, no single imaging technology can offer 100% detection of all early stage cancers. As such, if we are to offer women a method of true early detection, thermography, mammography, ultrasound, and MRI cannot be used alone. These are all adjunctive imaging technologies. Consequently, thermography’s role is in addition (an adjunct) to structural imaging and physical examination, not in lieu of. Thermography does not replace any other imaging technology, nor can any other imaging technology replace thermography. The tests complement each other. Since it has been determined that 1 in 8 women will get breast cancer, we must use every means possible to detect cancers when there is the greatest chance for survival. What we are promoting is a multimodal (multiple tests) approach to screening. The combined use of breast self-exams, physician exams, thermography, and structural imaging together provide the earliest detection system available to date [3,7-9]. If treated in the earliest stages, cure rates greater than 95% are possible [3,6]. With thermography’s expanded role as a risk assessment technology, infrared imaging brings a great deal of good news to women.
WHO SHOULD HAVE THIS TEST?
Every woman should include breast thermography as an addition to her regular breast health care. We must do everything we can to provide earliest detection in an effort to prevent women from having to deal with this terrible disease.
Breast cancers are particularly aggressive in younger women. Statistics indicate that approximately 15% of all breast cancers occur in women under the age of 45 [13]. However, there are no clear guidelines for the use of imaging procedures during these years. With the addition of breast thermography, women in this age group have a tool that they can add to their regular breast health check-ups.
Breast Thermography Guidelines
Initial infrared scan by age 20
20-30 years of age – every 3 years
30 years of age and over – every year
REFERENCES
- 1. American Cancer Society – Breast Cancer Guidelines and Statistics, 2009-2010
- 2. I. Nyirjesy, M.D. et al; Clinical Evaluation, Mammography and Thermography in the Diagnosis of Breast Carcinoma. Thermology, 1986; 1: 170-173.
- 3. M. Gautherie, Ph.D.; Thermobiological Assessment of Benign and Malignant Breast Diseases. Am. J. Obstet. Gynecol., 1983; V 147, No. 8: 861-869.
- 4. C. Gros, M.D., M. Gautherie, Ph.D.; Breast Thermography and Cancer Risk Prediction. Cancer, 1980; V 45, No. 1: 51-56.
- 5. P. Haehnel, M.D., M. Gautherie, Ph.D. et al; Long-Term Assessment of Breast Cancer Risk by Thermal Imaging. In: Biomedical Thermology, 1980; 279-301.
- 6. P. Gamigami, M.D.; Atlas of Mammography: New Early Signs in Breast Cancer. Blackwell Science, 1996.
- 7. J. Keyserlingk, M.D.; Time to Reassess the Value of Infrared Breast Imaging? Oncology News Int., 1997; V 6, No. 9.
- 8. P. Ahlgren, M.D., E. Yu, M.D., J. Keyserlingk, M.D.; Is it Time to Reassess the Value of Infrared Breast Imaging? Primary Care & Cancer (NCI), 1998; V 18, No. 2.
- 9. N. Belliveau, M.D., J. Keyserlingk, M.D. et al ; Infrared Imaging of the Breast: Initial Reappraisal Using High-Resolution Digital Technology in 100 Successive Cases of Stage I and II Breast Cancer. Breast Journal, 1998; V 4, No. 4
- 10. Verzini, L., Romani, L., Talia, B., (Radiology department university of Modena (Italy)). Thermographic variations in the breast during the menstrual cycle. Acta Thermographica, 143–149, 1980s.
- 11. Huber, C., Pons, J., Pateau, A., (Gynecology and department of radiology Cretei hospital (Paris) France). Breast fibrocystic disease and thermography. Acta Thermographica, 48–50, 1980s.
- 12. Borten, M., Ransil, B. et al. (Department of obstetrics and gynecology, Beth Israel Hospital, Harvard Medical School). Regional differences in breast surface temperature by liquid crystal thermography. Thermology, 1, 216–220, 1986.
- 13. American Cancer Society – Breast Cancer Guidelines and Statistics